Frequently Asked Questions About Jaw Fractures

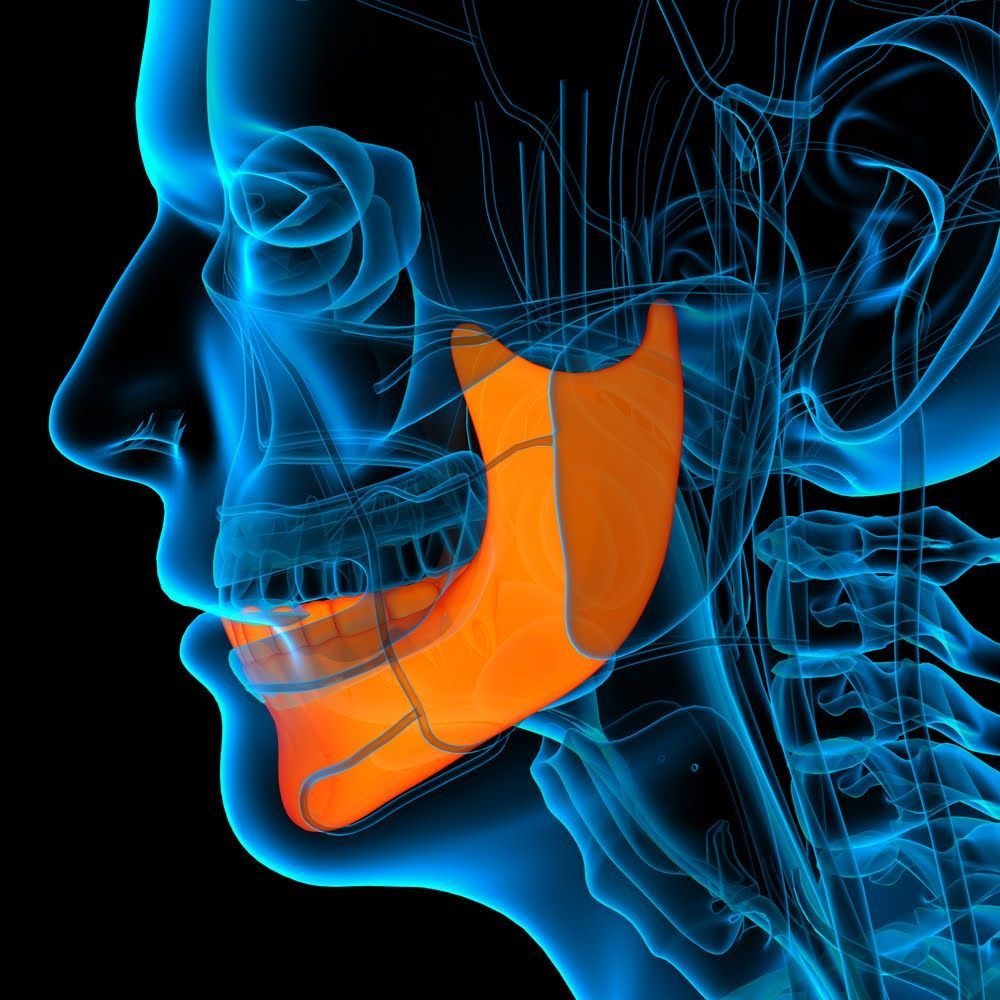
Fractures of the mandible, or lower jawbone, represent the third most common type of facial fracture and the tenth most common fracture overall. If you sustain this kind of fracture, you'll likely want a qualified maxillofacial specialist and/or oral surgeon to evaluate and treat your jaw.
A fractured jaw can prompt worry and confusion in sufferers. However, a strong basic understanding of what occurs in this condition and what doctors can do for it may ease your mind and help you take the right steps toward recovery. Check out these frequently asked jaw fracture questions.
Why Do Jaw Fractures Occur?
The mandible's prominent position in the lower front of the face naturally exposes it to injury risks. A strong, sudden impact can fracture this bone either along its main body or at its condyles, small knob-shaped bone ends that form part of the temporomandibular joints.
You can suffer a jaw fracture if someone punches you in the face, if you land on the ground face first, or if an auto accident throws your jaw into the steering wheel of your car. Assault injuries typically break the bone near the chin, while fall-related jaw fractures more commonly fracture the condyles.
What Symptoms May Indicate a Jaw Fracture?
When you first injure your jaw, you may wonder whether you have a full fracture, a dislocation, or both. Either type of injury can cause jaw pain, limited jaw motion, and trouble speaking or eating. However, fracture symptoms may also include loose teeth, swelling, numbness, and bleeding or bruising inside the mouth.
How Do Maxillofacial Specialists Treat a Fractured Jaw?
The first step in dealing with a fractured jaw involves thoroughly evaluating the damage. Maxillofacial specialists will examine your jaw's appearance, test your jaw function, look inside your mouth for other signs of injury, and check the alignment of your temporomandibular joints. X-rays or CT scans can reveal the fracture in detail.
Not all jaw fractures require surgical repair. If the pieces of your jaw remain in their usual positions, you may simply need to immobilize the jawbone long enough for it to heal on its own. An oral surgeon can achieve this goal by using fine wire to connect your upper teeth to your lower teeth. Open wounds may call for antibiotic treatment.
If your jaw fracture has caused more extensive damage or forced parts of the bone out of position, you may need surgery to realign, reattach, and stabilize the pieces. In a typical procedure, the oral surgeon anesthetizes you and then uses internal incisions to rejoin the bone fragments with metal screws and plates.
What Can You Expect During Your Jaw Fracture Recuperation?
You can expect a fractured jaw to require up to six weeks of healing time. During this period, you may have elastic bands attached to your teeth to keep the jaw from moving. You can reduce the swelling that occurs during the first couple of weeks by applying warm compresses on a regular schedule.
A sore throat often occurs as a normal temporary side effect of the general anesthetic you received. Bleeding from the nose or mouth merits more concern if it persists after your hospital stay, so you'll want to have your oral surgeon evaluate any such symptoms.
Self-care can prove a bit challenging during your recuperation from a broken jaw surgery. If you have had your jaw wired or banded shut, your oral surgeon can instruct you on how to prepare and ingest a liquid diet. Saline rinses may take the place of normal brushing during this time. Don't forget to keep your lips moisturized.
The San Diego Center for Oral & Maxillofacial Surgery can evaluate your fractured jaw and determine the proper course of treatment to ensure optimal healing. Contact our office to learn more about our jaw repair procedures and schedule an initial consultation.
Browse Our Website
Contact Information
Hours of Operation
- Mon - Thu
- -
- Friday
- -
- Sat - Sun
- Closed
Follow Us On: