Surgical Treatment for Sleep Apnea

Untreated sleep apnea can lead to excessive fatigue, high blood pressure, cardiovascular issues, and other serious complications.
Many sleep apnea patients are able to manage their conditions effectively by wearing a machine that helps maintain positive airway pressure, such as a CPAP or BiPAP. Other sleep apnea sufferers find relief with position changes during sleep, weight loss, or oral appliances worn during sleep.
Some people who have sleep apnea aren't able to wear a positive airway pressure device properly. If other treatments fail to resolve your apnea symptoms, you may want to consult with a facial surgeon to see if surgical intervention is right for you.
Pharyngoplasty
Uvulopalatopharyngoplasty, or UPPP, is the most common surgical procedure for sleep apnea. UPPP is usually recommended for patients who have obstructive sleep apnea and can't use a CPAP or other device to keep the airway open during sleep. A UPPP surgery involves the surgeon removing part of the uvula and soft palate. The edges of the soft palate and sides of the throat are then stitched together.
Other pharyngoplasty procedures may be better depending on what tissues and structures contribute to the patient's sleep apnea symptoms. Facial surgeons typically remove the tonsils during pharyngoplasty surgeries, and they may remove or reposition the soft tissue, uvula, and nearby tissues.
Nasal Surgery
Sleep apnea patients who have a nasal obstruction often require high CPAP pressure, which can be difficult to tolerate. A facial surgeon might suggest surgical intervention, such as a septoplasty, to help open the airways.
Enlarged tonsils and adenoids can also lead to sleep apnea, so surgery to remove them often helps improve symptoms, especially in children who suffer from sleep apnea.
Soft Palate Implants
Some sleep apnea patients can get relief from snoring and other mild sleep apnea symptoms from a minimally invasive procedure called the Pillar Procedure. During the Pillar Procedure, a surgeon implants three small rods into the soft palate. The rods cause the surrounding soft tissues to swell, which helps stiffen the soft palate. A stiff soft palate is less likely to reach the pharynx during sleep, which reduces snoring and apnea.
Hyoid Advancement
The hyoid bone in the neck where the tongue and pharynx attach can make airway obstruction more likely in sleep apnea patients who have a large tongue base. A surgeon may suggest a hyoid advancement surgery, which involves the surgeon relocating the hyoid bone by suspending it to the front of the patient's jaw. This surgery is minimally invasive with a quick healing time.
Tongue Surgery
Many sleep apnea patients stop breathing during sleep due to the tongue falling backward, which blocks the airway. A surgeon can move the genioglossus muscle in the tongue forward so it can't fall back as easily while the patient is asleep.
Some sleep apnea patients also benefit from having the base of their tongues reduced. This can be done with radio waves that help shrink the tissue at the base of the tongue without affecting the surrounding tissue. A portion of the tongue tissue at the base can also be moved directly through surgery.
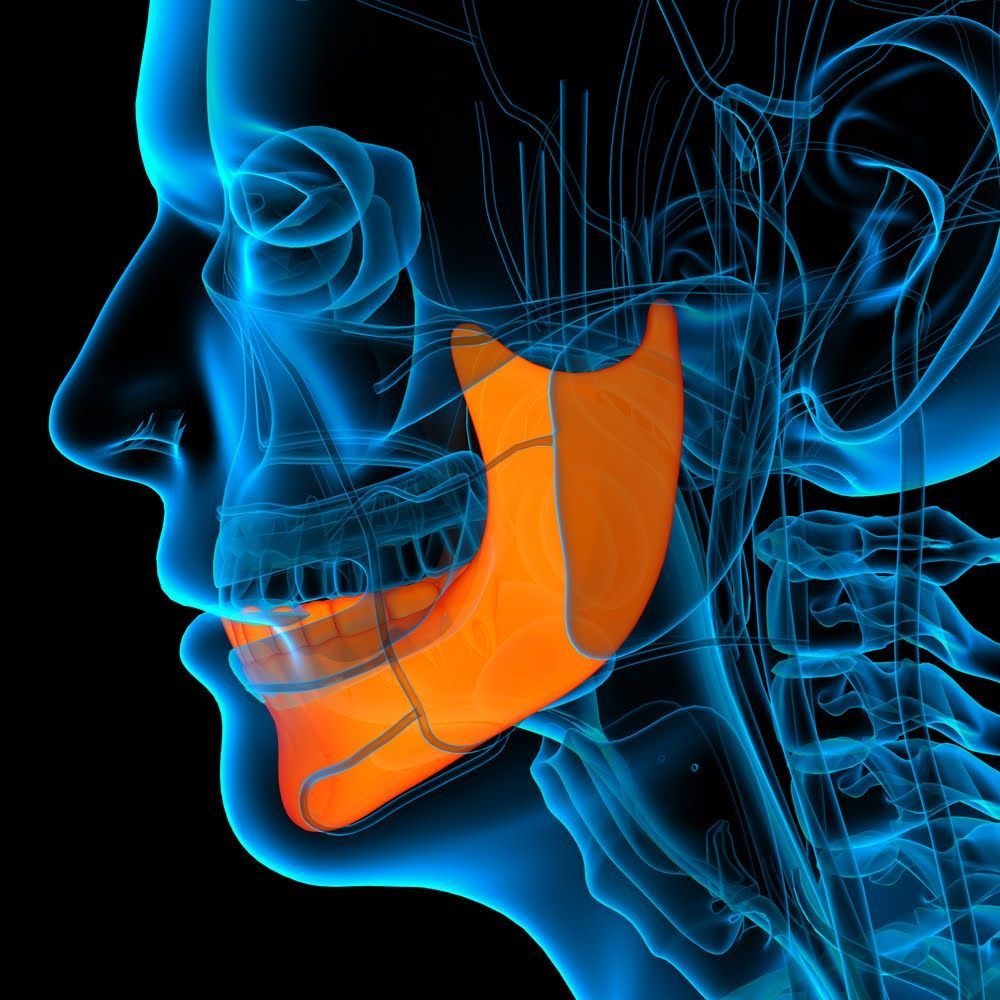
Jaw Advancement
The position of the jaw can make sleep apnea more likely in some patients, so surgery to reposition the jaw can be effective for some people. The upper and lower jaw are advanced during a surgical procedure, which opens the upper airway. The jaws are stabilized with titanium after they are repositioned.
Jaw advancement surgery is more invasive than many other treatments, and patients often have a long healing time, so jaw surgery is typically a last resort.
The San Diego Center for Oral & Maxillofacial Surgery is a fully-equipped oral surgery center with staff who specialize in dental implants, oral surgery, and reconstructive facial surgery. If you have sleep apnea and want to explore your treatment options,
contact us today to schedule an appointment with one of our experienced oral surgeons.
Browse Our Website
Contact Information
Hours of Operation
- Mon - Thu
- -
- Friday
- -
- Sat - Sun
- Closed
Follow Us On: